Post-Exposure Prophylaxis (Pep) in Kenya
Post-exposure prophylaxis, also known as post-exposure prevention (PEP), is any preventive medical treatment started after exposure to a pathogen to prevent the infection from occurring.
PEP (post-exposure prophylaxis) means taking antiretroviral medicines (ART) after being potentially exposed to HIV to prevent becoming infected. The PEP should be used only in emergencies and must be started within 72 hours after recent possible exposure to HIV.
Initiation of post-exposure prophylaxis with the use of antiretroviral drugs is dependent on several risk factors, though treatment is usually started after one high-risk event. To determine whether post-exposure prophylaxis is indicated, an evaluation visit will be conducted to consider risk factors associated with developing HIV. Assessments at this visit will include whether the at-risk person or the potential source-person are HIV positive, details around the potential HIV exposure event, including timing and circumstances, whether other high-risk events have occurred in the past, testing for sexually transmitted diseases, testing for hepatitis B and C (nPEP is also effective against hepatitis B), and pregnancy tests for women of childbearing potential.
Risk factors for developing HIV include exposure of mucous membranes (vagina, rectum, eye, mouth, broken skin, or under the skin) of an HIV-negative person to bodily fluids (blood, semen, rectal secretions, vaginal secretions, breast milk) of a person known to be HIV positive. For example, having unprotected sex with HIV positive partner is considered risky, but sharing sex toys, spitting, and biting are considered to be negligible risks for initiating post-exposure prophylaxis. The highest non-sexual risk is blood transfusion and the highest sexual contact risk is receptive anal intercourse. The timing of exposure does not affect the risk of developing HIV, but it does alter whether post-exposure prophylaxis will be recommended. Exposures that occurred 72 hours or less to the beginning of treatment are eligible for post-exposure prophylaxis. If the exposure occurred over 73 hours before treatment initiation, post-exposure prophylaxis is not indicated.
Before initiating PEP after potential HIV exposure, persons should be tested for HIV1 and HIV2 antigens and antibodies in the blood using a rapid diagnostic test. The PEP should only be started if a rapid diagnostic test reveals no HIV infection present or if tests results are not available. However, if HIV infection is already present then PEP should not be started. HIV test should be repeated four to six weeks and three months after exposure.
Non-occupational exposures include cases when a condom breaks while a person with HIV has unprotected sex with an HIV-negative person in a single incidence, or the case of unprotected sex with an anonymous partner, or in the case of a non-habitual incident of sharing a syringe for injection drug use. Evidence suggests that PEP also reduces the risk of HIV infection in these cases.
Occupational exposures include needlestick injury of health care professionals from an HIV-infected source.
PEP drugs in Kenya | PEP regimen in Kenya | Medication | PEP Dosage
Three-drug PEP regimens are now the recommended regimens for all exposures owing to the safety and tolerability of new HIV drugs. The guidelines no longer require assessing the severity of the exposure. There are some special circumstances, however, in which a 2-drug regimen can be used, especially when recommended antiretroviral medications are unavailable or there is concern about potential adherence problems or toxicity. An expert should be consulted if a 2-drug PEP regimen is being considered.
The preferred HIV 3-drug PEP regimen is raltegravir (I 400 mg PO twice daily plus Truvada® (tenofovir DF 300 mg/emtricitabine 200 mg) 1 PO once daily
The 2016 guidelines for antiretroviral postexposure prophylaxis for nonoccupational exposure to HIV recommend either raltegravir (RAL) 400 mg twice daily or dolutegravir (DTG) 50 mg daily in combination with tenofovir disoproxil fumarate (TDF) 300 mg and emtricitabine (FTC) 200 mg daily as the preferred regimen in healthy adults and adolescents. Dolutegravir provides a reasonable once-daily alternative to raltegravir. This ART regimen is not in the 2013 post-occupational exposure to HIV guidelines since it was FDA-approved after the PEP guidelines were written but are favored by most authorities. However, recent data suggest an increased risk of neural tube defects associated with exposure to dolutegravir (DTG) at conception. Based on these preliminary data, the CDC has updated occupational and nonoccupational recommendations while the data undergo further review.
The CDC recommends that healthcare providers avoid DTG for PEP in the following patients:
Nonpregnant women of childbearing potential who are not on an effective birth control method who are sexually active or who have been sexually assaulted
Pregnant women who are early in their pregnancy (within the first 28 days)
In these situations, the preferred PEP regimen is raltegravir, tenofovir, and emtricitabine.
The PEP should be taken for 28 days. It is important to take all the doses, at the right time and in the right way, to give PEP the best chance of working. You might be given an additional two days of drugs if you have been at risk of exposure in the last 48 hours of the course of PEP.
PEP Side Effects:
As with most antiretroviral drugs, PEP can cause side effects such as diarrhea, headaches, nausea/vomiting, and fatigue. However, these are usually mild and generally only last a few days with no long-term side effects.
In rare cases, they can cause serious health issues, including liver problems.
PEP in Kenya hospitals | pep availability in Kenya | How to access pep in Kenya
You can get PEP in all major public, and private hospitals and VCT Centers Countrywide.
PEP price in Kenya pep cost in Kenya
In Kenya PEP is found in a government hospital for free.
Some private hospitals such as Nairobi Women’s hospital provide PEP for free.
How effective is the PEP
PEP is effective in preventing HIV when administered correctly, but not 100%.
It is most effective when started within 24 hours, but it needs to be started within 72 hours. The longer you wait, the greater the chance that PEP won’t work. PEP usually isn’t given more than 72 hours (3 days) after exposure as studies show it is unlikely to be effective.
How does PEP work
PEP works by stopping the virus from replicating after recent exposure. The cells originally infected with HIV die naturally within a short period, reducing the likelihood for HIV to establish itself in the body.
can you get PEP over the counter?
No, You cannot get PEP over the counter.
Why does PEP fail?
PEP failure, when it occurs, is usually attributed to delayed initiation, transmitted drug resistance, or suboptimal medication adherence.
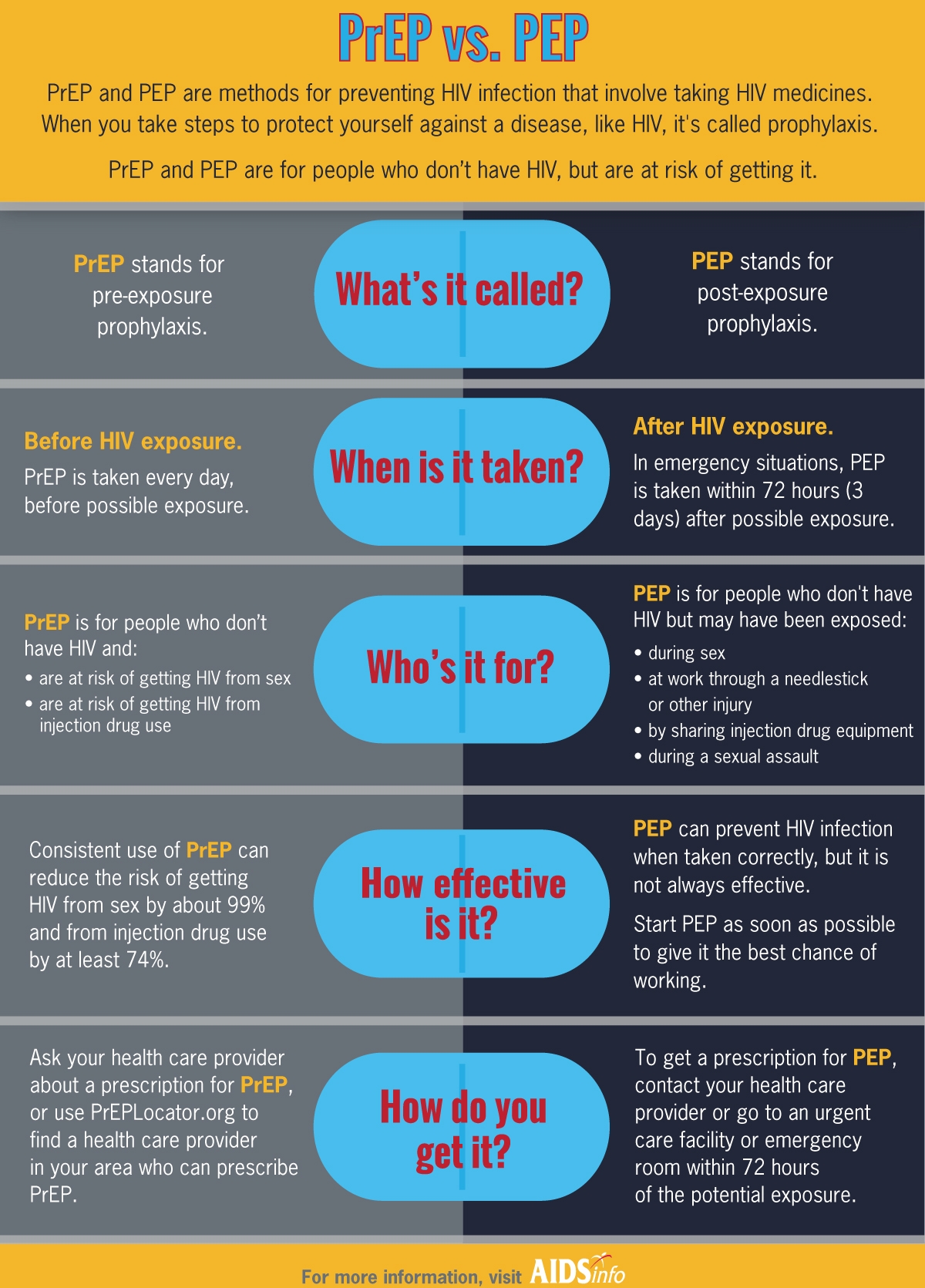
Difference between PrEP and PEP
Drugs used as PrEP
Pre-exposure prophylaxis (PrEP) is a course of HIV drugs taken by HIV-negative people to protect them against HIV infection. Truvada is currently the only drug approved for use as PrEP. Truvada is a single pill that is a combination of two anti-HIV drugs, tenofovir, and emtricitabine.
See Also:
vct centres in Nairobi